Heller’s myotomy
Achalasia Cardia Treatment
Know About
What is Achalasia Cardia?
Elce clinic provide the best achalasia cardia treatment. Achalasia affects the esophagus, the tube that carries swallowed food from the back of the throat down into the stomach. A ring of muscle called the lower esophageal sphincter encircles the esophagus just above the entrance to the stomach. This sphincter muscle is normally contracted to close the esophagus. When the sphincter is closed, the contents of the stomach cannot flow back into the esophagus. Backward flow of stomach contents (reflux) can irritate and inflame the esophagus, causing symptoms such as heartburn.
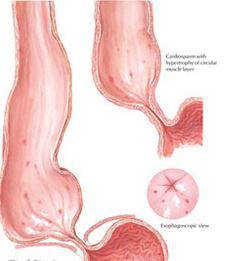
We are the Best Achalasia cardia treatment providers. The act of swallowing causes a wave of esophageal contraction called peristalsis. Peristalsis pushes food along the esophagus. Normally, peristalsis causes the esophageal sphincter to relax and allow food into the stomach. In achalasia, which means ❝failure to relax❞, the esophageal sphincter remains contracted. Normal peristalsis is interrupted and food cannot enter the stomach.
What causes Achalasia Cardia?
Achalasia is caused by degeneration of the nerve cells that normally signal the brain to relax the esophageal sphincter. The ultimate cause of this degeneration is unknown. Autoimmune disease or hidden infection is suspected. Theories reveal that genetics, abnormal immune system, infection etc may cause achalasia cardia. The most accepted theory is the imbalance in the neurotransmitters. The esophageal nerves fail to create peristalsis movements in the esophageal muscles and the lower esophageal sphincter. This causes difficulty in swallowing.

What are the symptoms?
Dysphagia, or difficulty swallowing, is the most common symptom of achalasia. The person with achalasia usually has trouble swallowing both liquid and solid foods, often feeling that food “gets stuck” on the way down. The person has chestpain that is often mistaken for cardiac pain. Heart burn and difficulty belching are common. usually this condition gets steadily worse. Other symptoms may include nighttime cough or recurrent pneumonia caused by food passing into the lower airways.
Diagnosis
Diagnosis of achalasia begins with a careful medical history. The history should focus on the timing of symptoms and one eliminating other medical conditions that may cause similar symptoms. Endoscopy. In this test, a tube containing a lens and a light source is passed into the esophagus. Endoscopy is used to look directly at the surface of the esophagus. This test can also detect tumors that cause symptoms like those of achalasia. Cancer of the esophagus occurs as a complication of achalasia in 2-7% of patients. The diagnostic tests involved to diagnose Achalasia Cardia are Barium Swallow X-Ray, Esophageal Manometry, Endoscopy of the Esophagus, Stomach, and Duodenum. Achalasia Cardia will be diagnosed if food particles are found above the lower esophageal sphincter in endoscopic diagnosis.
How is cholecystitis diagnosed?
Diagnosing cholecystitis starts when you describe your symptoms to your doctor. Next is a physical exam. Your doctor will carefully feel your right upper abdomen to look for tenderness. You may have blooddrawn and an ultrasound, a test that uses sound waves to create a picture of your gallbladder. Ultrasound may show gallstones, thickening of the gallbladder wall, extra fluid, and other signs of cholecystitis. This test also allows doctors to check the size and shape of your gallbladder.
Achalasia Cardia Treatment
Surgical options – Heller’s Myotomy
A surgical procedure called the Heller myotomy has become the treatment of choice and offers long-term symptomatic relief to those who have the disorder. This procedure weakens the muscles at the gastroesophageal junction, allowing the valve between the esophagus and stomach to remain open. Although there is no definitive medical treatment, medical therapies may help to relieve the symptoms of achalasia in its early stages.
Several treatment procedures are available for achalasia but these nonsurgical and surgical treatments cannot bring the normal (peristaltic) contractions of the esophagus. These treatment weakens the lower esophageal sphincter that can just allow the flow of food without becoming as a barrier for the passage of food. There are two ways of treatment for weakening the esophagus muscle such as nonsurgical drug therapy and surgical treatment where the LES muscle is cut down.
Non Surgical Treatments
Pneumatic Dilation:
- In this procedure the balloon is inserted into the lower esophageal sphincter(LES) and expanded to enlarge the opening.
- The procedure of expanding the LES is repeated if it is not properly stay open and difficulty in the flow of food.
- The patient has to repeat their treatment within six years that weakness the LES muscle.
Botox Injection:
- Botox is a muscle relaxant drug which can be injected using endoscope directly into the esophageal sphincter.
- The procedure of injecting the botox is repeated that make the muscle of LES to relax.
- The disadvantage of this procedure is repeating the injection can weaken the muscle that becomes difficult for the surgery later if needed any.
- The procedure is performed for the patients who cannot support the pneumatic dilation, age or lack in overall fitness.
Medication:
- The achalasia cardia surgeon suggest the muscle relaxant drug such as nitroglycerin (nitrostat) or nifedipine (procardia) to weaken the LES muscle.
- This procedure has a limited treatment effect and also reflects severe side effects.
- The procedure is performed for the patients who aren’t good for dilation, botox injection and surgical treatments.
Surgical Treatments
The surgical achalasia cardia treatment is recommended for younger people because the non- surgical treatment is ineffective for them.
Heller Mytomy:
- Heller mytomy is a procedure where the lower esophagus sphincter muscle is cut to allow the food to pass smoothly into the stomach.
- This procedure is performed as a laparoscopic heller mytomy where the surgeon cuts the muscle using the laparoscope incision.
- There is a possibility of the gastroesophageal reflux disease (GERD) developed after the heller mytomy procedure.
Fudoplication:
- The surgeon wraps top of the stomach around the lower esophageal sphincter which tightens the muscle and also prevents acid reflux.
- Fudoplication surgery is performed at the same time along with heller mytomy procedure to avoid the GERD problem in the future.
- The Fundoplication is performed as the laparoscopic procedure where the camera is inserted through a small incision made by laparoscope and wrap the stomach using the device at the other end.
Peroral Endoscope Myotomy(POEM):
- In this procedure the surgeon uses the endoscope which is inserted through mouth and down through the throat to provide an incision lining the esophagus and cut the muscle like heller mytomy procedure.
- But in POEM doesn’t include the anti-reflux procedure that leads to GERD in the future.
